What affects your mood? Are you fatigued, sleep-deprived and depressed? #ClinicSpeak #MSResearch #MSBlog Are #GroupClinics the solution?
Edwards et al. The Relative Importance of Baseline Pain, Fatigue, Sleep and Physical Activity: Predicting Change in Depression in Adults with Multiple Sclerosis. Archives of Physical …, 2016. DOI: http://dx.doi.org/10.1016/j.apmr.2016.02.025
Design: Observational longitudinal survey study.
Setting: A community-based population sample.
Participants: Adults with multiple sclerosis (MS; N = 489).
Interventions: Not applicable.
Main Outcome Measures: Primary outcome was classification of depression group measured using a PHQ-9 cut-off score of ≥ 10, indicating probable major depression.
Results: Fatigue severity (odds ratio, 1.19, 95% confidence interval, 1.12 – 1.26, P < .0001) and sleep disturbance (odds ratio, 1.06, 95% confidence interval, 1.02 – 1.10, P = .001) predicted probable major depression 3.5 years later among those not depressed at the initial assessment. An effect of age (odds ratio, 0.96, 95% confidence interval, 0.92 – 0.99, P = .008) was found among those who developed depression, indicating that younger adults were more likely to develop depression. Pain, fatigue, sleep, and physical activity at baseline were not significantly associated with recovery from depression among those depressed at the initial assessment.
Conclusions: Fatigue and sleep may contribute to the development of depression. Clinical trial research targeting these variables to determine their influence on depression is warranted.
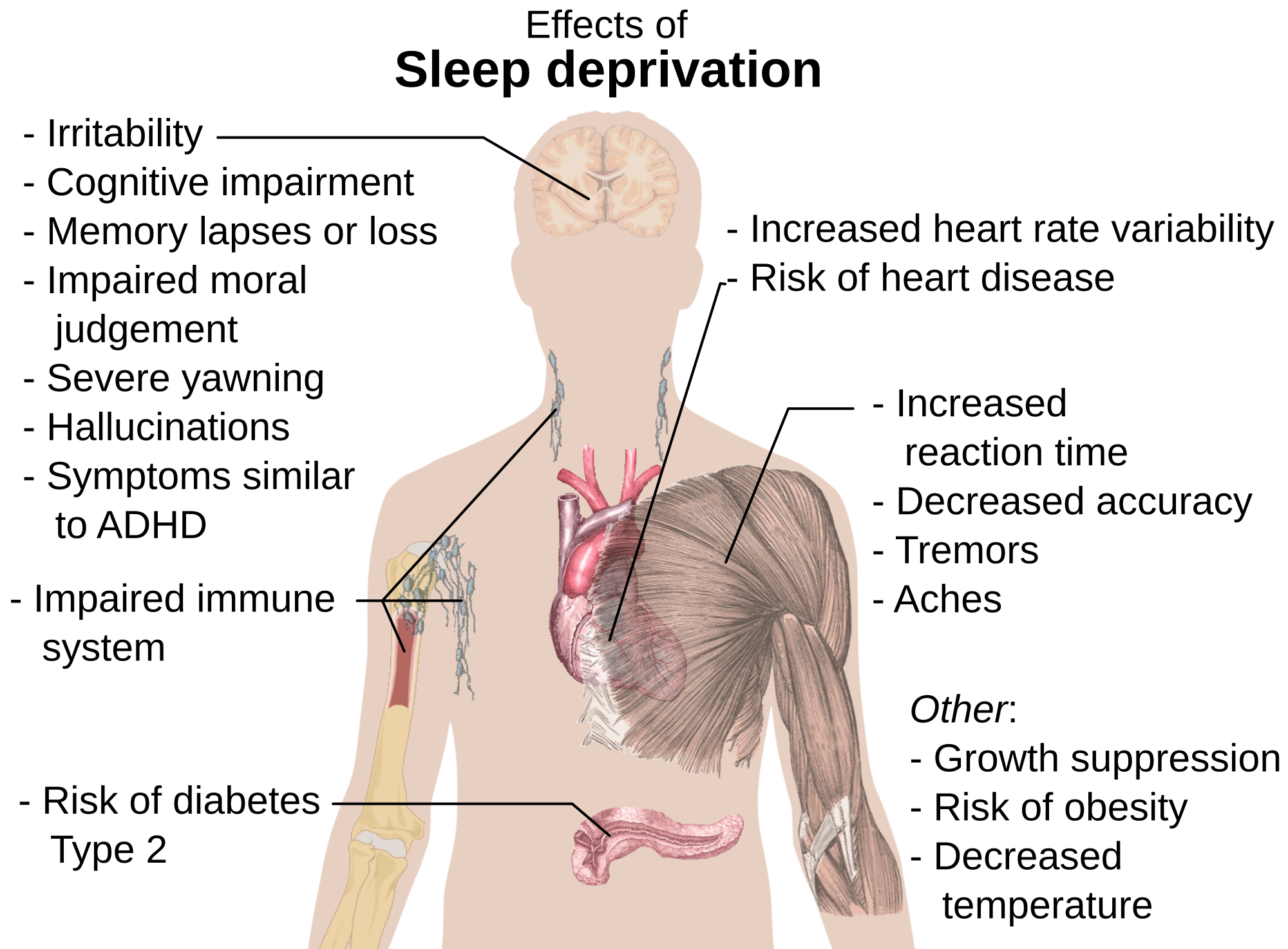
“The study below demonstrates that fatigue and sleep disturbances predict the development of depression in MSers at follow-up a few years down the line. I am not surprised by this study’s findings the brain responds to all complex percepts (integrated sensory perceptions) with an affective response, or a change in mood. What I mean is that if you are fatigued it is natural for you to feel low or depressed; fatigue is generally a negative symptom and you respond with a lowering of your mood. Fatigue and depression go hand-in-hand. Sleep disturbance is also related to the two problems. Not sleeping properly is very common in MSers and relates to many different, and varied, causes and is one of the main drivers of fatigue. Therefore it is not surprising that MSer who are sleep-deprived and don’t get good quality deep sleep, feel fatigued and depressed. I am sure many of you relate to these problems.”
“For many reasons, some of which are highlighted above, we are planning to start a trial of group clinics to target sleep disorders in MSers. We simply don’t have enough time in the NHS-allocated 15 minute follow-up slots to manage your sleep problems properly. We are therefore asking 12 MSers to pool their 15 minutes slots to give us 3 hours during which we tackle sleep problems as a group. By doing this we can teach you about sleep disorders in MS get you to self-diagnose your problems and self-manage them with the help of the group. Group clinics are not new and have been used in psychiatry for decades and have more recently been shown to improve outcomes in other chronic diseases. The question is are you prepared to share your time with others and speak about your problems with others? I suspect group clinics is not the answer for everyone. Are you prepared to try being part of the experiment?”
Edwards et al. The Relative Importance of Baseline Pain, Fatigue, Sleep and Physical Activity: Predicting Change in Depression in Adults with Multiple Sclerosis. Archives of Physical …, 2016. DOI: http://dx.doi.org/10.1016/j.apmr.2016.02.025
Objective: To determine if baseline levels of pain, fatigue, sleep disturbance and physical activity measured at the initial assessment predicted the development of or improvement of depression 3.5 years later, while controlling for sex, age, and disease severity. This research is important, as few studies have examined these modifiable factors using a longitudinal design.
Design: Observational longitudinal survey study.
Setting: A community-based population sample.
Participants: Adults with multiple sclerosis (MS; N = 489).
Interventions: Not applicable.
Main Outcome Measures: Primary outcome was classification of depression group measured using a PHQ-9 cut-off score of ≥ 10, indicating probable major depression.
Results: Fatigue severity (odds ratio, 1.19, 95% confidence interval, 1.12 – 1.26, P < .0001) and sleep disturbance (odds ratio, 1.06, 95% confidence interval, 1.02 – 1.10, P = .001) predicted probable major depression 3.5 years later among those not depressed at the initial assessment. An effect of age (odds ratio, 0.96, 95% confidence interval, 0.92 – 0.99, P = .008) was found among those who developed depression, indicating that younger adults were more likely to develop depression. Pain, fatigue, sleep, and physical activity at baseline were not significantly associated with recovery from depression among those depressed at the initial assessment.
Conclusions: Fatigue and sleep may contribute to the development of depression. Clinical trial research targeting these variables to determine their influence on depression is warranted.
I have just been on a sleep matters course, in a group and face to face aimed at those with mild to moderate mental health issues. It did highlight the link of anxiety, depression and stress with sleep issues. I thought it was very relevant to my MS and some other people on the course suffered from various health conditions.
I would be happy to pool my MS nurse appointment time but not time with my neurologist. I get to see him so rarely. I think possibly an online group MS sleep clinic could be of value. I would sign up for it.
Im not a patient there, but want to offer a bit of experience. A couple years ago, I participated in a group research study on fatigue for MSers. One of our group seemed to have cognitive problems and didn't pick up social cues well. She dominated discussion and soaked up valuable interaction time by giving everyone advice–at length. If I did something like that again, I would hope for group leaders who are more skilled at managing situations like that.
I have been on a few courses like that and there is always a person who likes the sound of their own voice. One course there was a person with verbal diarrhoea and mumbling. The course facilitator was struggling to stop them talking. The other course like anon above a participant gave constant advice.
Agree with anon 11.40 that an online group could work and may be preferable – allowing for people who are not local to your clinic and also to keep response time/volume to a manageable level
Sleep deprivation and chronic conditions is the BBC news site today.http://www.bbc.co.uk/news/health-35945133