#MSBlog: Is Prof G recommending too much vitamin D?
Holmøy T, Torkildsen O, Myhr KM, Løken-Amsrud KI. Vitamin D supplementation and monitoring in multiple sclerosis: who, when and wherefore. Acta Neurol Scand Suppl. 2012;(195):63-9. doi: 10.1111/ane.12028
OBJECTIVES: Observational studies suggest that increasing the serum concentration of 25-hydroxyvitamin D by 50nmol/L could halve the relapse risk in RRMSers. Assuming that the association between disease activity and vitamin D status is entirely causal may however exaggerate the potential benefit. The aim of this paper is to address whether and how vitamin D should be monitored in MSers.
METHODS: Possible benefits of vitamin D supplementation were assessed from observational, experimental and clinical studies. Based on repeated measurements of 25-hydroxyvitamin D in Norwegian MSers , they estimated the effect of different supplementation regimes.
RESULTS: Serum levels of 25-hydroxyvitamin in the upper physiological range are associated with lower risk of relapses and magnetic resonance imaging disease activity, but the causality is uncertain. Osteoporosis or oseteopaenia (thin bones) develops early in MS , and 25-hydroxyvitamin vitamin should therefore at least be 50 nmol/L throughout the year. Levels between 75 and 125 nmol/L may offer some additional benefit for bone health, are not toxic and are associated with low disease activity. Adding 400 IU (10 μg) vitamin D daily would only bring 56% of the patients >50 nmol/L and 11% >75 nmol/L throughout the year, whereas 800 IU (20 μg) would maintain 97% >50 nmol/L and 67% >75 nmol/L.
CONCLUSION: We recommend that MS patients are supplemented with 800 IU of vitamin D at least from autumn to spring. Alternatively, 25-hydroxyvitamin D should be measured and the nadir level estimated and supplementation given to a target level between approximately 75 and 125 nmol/L.
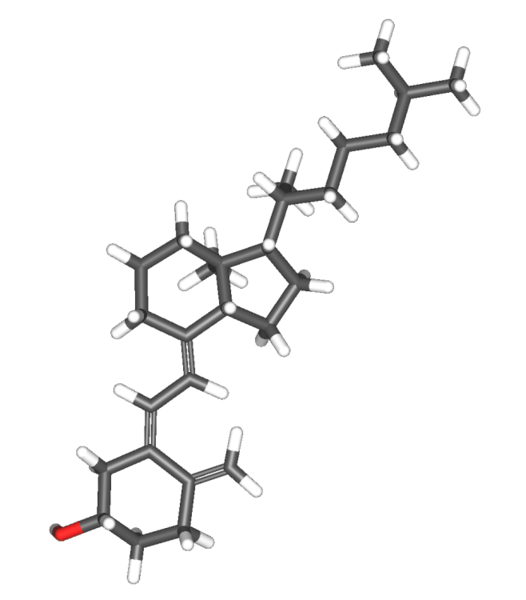 |
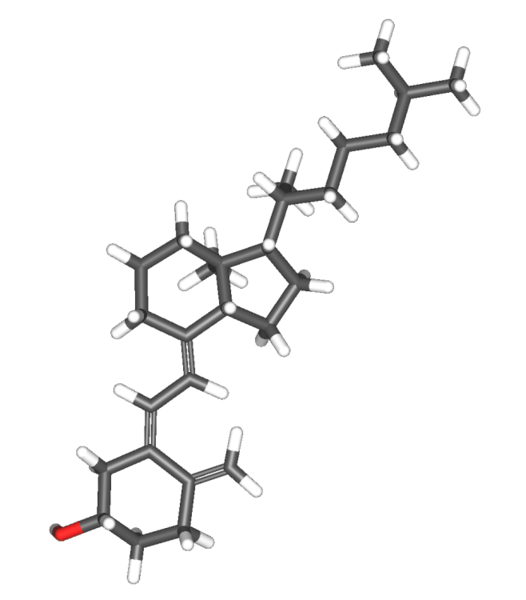
| Vitamin D |
“This vitamin D experts are staying that when you look at ancestral populations, for example hunter-gatherer societies and populations living outdoors in the tropics, they don’t have a cyclical pattern of vD levels, i.e. high levels at the end of summer and low levels at the end of winter and their levels remain well above 100nmol/L all year round. These populations don’t get MS either. Therefore some experts have been recommending that we aim for constant levels above 100nmol and no cycling of levels; this is what we would call ancestral physiological vitamin D level supplementation. This is why wee have been recommending 5,000U vD3 per day for adults and 10,000U vD3 per day for woman planning to fall pregnant and who are pregnant. Please note vD supplements should not be taken with calcium supplements as this can result in hypercalcaemia or high blood calcium levels. These levels of supplementation are not far off the recent European guidelines.”
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA); Scientific Opinion on the Tolerable Upper Intake Level of vitamin D. EFSA Journal 2012;10(7):2813. [45 pp.] doi:10.2903/j.efsa.2012.2813.
NEW RECOMMENDED DAILY ALLOWANCES FOR VITAMIN D3 SUPPLEMENTATION
- Adults 18 years or older = 4,000 U/day or 100 micrograms/day
- Children 11-17 years of age = 4,000 U/day or 100 micrograms/day
- Children 1-10 years of age = 2,000 U/day or 50 micrograms/day
- Infants less than 1year of age = 1,000 U/day or 25 micrograms/day
- Maximum safe dose or NOAEL = 11,000 U/day or 275 micrograms/day
Other vD posts of interest:
22 Jun 2012
CONCLUSION: In this study, IFN-β therapy is associated with greater production of vitamin D from sun exposure, suggesting part of the therapeutic effects of IFN-β on relapse in MS may be through modulation of vitamin D …
17 Jun 2012
Monthly moving averages of 25-OH-D levels were categorized into low (<50 nmol/L), medium (50-100 nmol/L), and high (>100 nmol/L) levels. Exacerbation risk decreased significantly with higher serum vitamin D levels: …
25 Aug 2012
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA); Scientific Opinion on the Tolerable Upper Intake Level of vitamin D. EFSA Journal 2012;10(7):2813. [45 pp.] doi:10.2903/j.efsa.2012.2813. Following a request …
01 Jun 2012
For adults, the 5-microg (200 IU) vitamin D recommended dietary allowance may prevent osteomalacia in the absence of sunlight, but more is needed to help prevent osteoporosis and secondary hyperparathyroidism.
12 Oct 2012
BACKGROUND:Low levels of plasma 25-hydroxyvitaminD (25(OH)D) are associated with a higher incidence of multiple sclerosis (MS) due to the immune suppressive properties of vitamin D.The aim of this study was to …
14 Oct 2012
When you have a group meeting ask how much vitamin D you are taking and who has been relapsing you will get idea if there are more than 12 of you then if right loads should have had problems. We have to wait for the …
06 Sep 2012
In last week’s BMJ there was a short article that suggested that low vitamin D levels could be a consequence rather then the cause of disease. The investigators’ showed that when someone is admitted to hospital and have a …
02 Sep 2012
I am convinced by the Vitamin D argument and hope that neurologists the country over recommend this to their patients. A few questions though: 1. Has Vitamin D levels in people with PPMS been studied? It seems the …
10 Aug 2012
What is needed to keep persons with multiple sclerosis vitamin D-sufficient throughout the year? J Neurol. 2012 Aug. Vitamin D sufficiency has been associated with lower risk of MS and may also
17 Aug 2012
Objective: Vitamin D deficiency and Epstein-Barr virus (EBV) infection may be associated with the development of MS. We investigated serum 25-hydroxyvitamin D (25-OH-D) levels and anti-EBV immunoreactivity in 25 …
27 Jul 2012
Contributions of vitamin D response elements and HLA promoters to multiple sclerosis risk. Neurology. 2012 Jul 11. “This research is what I call hard-core functional genomics and supports other studies already published.
23 Jul 2012
Research: predicting vitamin D levels. Epub: Saltytė Benth et al. Modelling and Prediction of 25-Hydroxyvitamin D Levels in Norwegian Relapsing-RemittingMultiple Sclerosis Patients. Neuroepidemiology. 2012 Jul …
12 Aug 2012
Vitamin D Responsive Elements within the HLA-DRB1 Promoter Region in Sardinian Multiple Sclerosis Associated Alleles. PLoS One. 2012;7(7):e41678. “This is hardcore science and looks at the interaction of vD with the …
20 Jul 2012
RESULTS: In 76 patients, immunomodulatory therapy preceded vitamin D supplementation (by 4.2 ± 2.7 years) and in 80 patients both treatments were started simultaneously. Under supplementation, the 25-OH-D level …
09 Jul 2012
“This study shows that it is not just MS that links with month of birth and further indicates that at some stage we are going to have make sure that pregnant woman are vitamin D replete througout pregnancy. This is perhaps …
12 Jul 2012
More evidence for Vitamin D? Fragoso YD et al. Month of Birth Does Not Seem to Interfere with the Development of Multiple Sclerosis Later in Life in Brazilian Patients. Neuroepidemiology. 2012 ;39(1):70-71. [Epub ahead of …
22 Jun 2012
CONCLUSION: In this study, IFN-β therapy is associated with greater production of vitamin D from sun exposure, suggesting part of the therapeutic effects of IFN-β on relapse in MS may be through modulation of vitamin D …
17 Jun 2012
Monthly moving averages of 25-OH-D levels were categorized into low (<50 nmol/L), medium (50-100 nmol/L), and high (>100 nmol/L) levels. Exacerbation risk decreased significantly with higher serum vitamin D levels: …
25 Aug 2012
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA); Scientific Opinion on the Tolerable Upper Intake Level of vitamin D. EFSA Journal 2012;10(7):2813. [45 pp.] doi:10.2903/j.efsa.2012.2813. Following a request …
01 Jun 2012
For adults, the 5-microg (200 IU) vitamin D recommended dietary allowance may prevent osteomalacia in the absence of sunlight, but more is needed to help prevent osteoporosis and secondary hyperparathyroidism.
24 May 2012
The development of experimental autoimmune encephalomyelitis (EAE), a model of multiple sclerosis, has been studied in mice that were (i) vitamin D-deficient, (ii) minus the vitamin D receptor, (iii) minus a vitamin D …
29 May 2012
Higher vitamin D levels were associated with lower, but not statistically significant, relapse risk. Except for the EDSS model, all associations were stronger when the within-person change in vitamin D level was the predictor.
22 May 2012
Vitamin D levels in Hispanics with multiple sclerosis. J Neurol. 2012 May Background: Vitamin D has been associated with MS and several markers of disease state in whites. There are limited reports of vitamin D’s influence in …
01 Jun 2012
Research: Vitamin D receptor and MS. Epub: Disanto et al. Vitamin D receptor binding, chromatin states and association with multiple sclerosis. Hum Mol Genet. 2012 May 16. Both genetic and environmental factors contribute …
05 Jul 2011
In this study there is a link between hospital admissions due to MS in Scotland and the average vitamin D levels in the previous 4 months. As you can see from the graphs above the greatest admission rates were in Spring …
06 Feb 2012
The associations between different sun exposure habits/vitamin D levels and MS were calculated as odds ratios (OR) with 95% confidence intervals (CI) using logistic regression. Potential interaction was evaluated by …
28 Dec 2012
Walton Centre; who gave us both the history of research findings re vitamin D & MS, and showed 5 recent studies where administration of high dose vit D ( 3, except for 1 study) did not show any effect on disease activity at all.
23 Feb 2012
Background: High vitamin D levels may reduce the risk of relapses and disease progression in MS. Methods: This 96-week randomised controlled trial was designed to assess the effect of vitamin D3 supplementation on bone …
23 Feb 2012
Background: High vitamin D levels may reduce the risk of relapses and disease progression in MS. Methods: This 96-week randomised controlled trial was designed to assess the effect of vitamin D3 supplementation on bone …
17 Jul 2011
The main source of vitamin D for Australians is exposure to sunlight. Thus, levels of blood vitamin D levels vary according to the season and are lower at the end of winter. In Australia and New Zealand, the number of people …
10 Mar 2012
Results: Median change in BOD was 287 mm(3) in the placebo group and 83 mm(3) in the vitamin D group (p=0.105). Serum levels of 25(OH)D increased from a mean of 54 (range 19-82) nmol/l to 110 (range 67-163) nmol/l …
05 Jul 2011
We need sufficient amount of sunlight exposure to synthesis our body’s requirement of vitamin D; this does not happen in Britain and many parts of the world. Change in behaviours is contributing to vitamin D deficiency: …
Like this:
Like Loading...
So are you saying now that we should take 4000 instead of 5000 iu's a day? Is it a problem to take 5000iu's? I'm saying this as I don't think the neutriceutical companies produce 4000iu capsules. So it means buying 1000 or 2000 and taking more capsules which ends up more expenive than just one 5000 iu capsule.
There is little difference between 4,000 and 5,000U per day. Therefore, I still recommend what the Vitamin D Council says; i.e. at least 5,000U per day. Vitamin D Council recommended amounts:Based on the body's indicated daily vitamin D usage, Vitamin D Council recommends the following amounts of supplemental vitamin D3 per day in the absence of proper sun exposure. Due to the variable response discussed above, these are only estimated amounts.Healthy children under the age of 1 years – 1,000 IU.Healthy children over the age of 1 years – 1,000 IU per every 25 lbs of body weight.Healthy adults and adolescents – at least 5,000 IU.Pregnant and lactating mothers – at least 6,000 IU.Additionally, children and adults with chronic health conditions such as autism, MS, cancer, heart disease, or obesity may need as much as double these amounts.The 5,000U tablets are much cheaper than purchasing 4 x 1,000U tablets. I do practice what I preach; my whole family and I are on 5,000U vD3 per day (summer and winter) and I purchase our tablet via the Vitamin D Council's website.
http://www.vitamindcouncil.org/about-vitamin-d/how-to-get-your-vitamin-d/vitamin-d-supplementation/
Firstly they cannot even get the units right it is nmol per something. If they cannot get this correct how can I trust the rest of their work. As the vitamin d being taken is not active any not used will be disposed of as 25(OH)D has a half life of 20 to 30 days. So 4000IU or 5000IU a day make no difference, even 11,000IU a day has a very large safety margin.
by convention nmol is per litre; I have therefore edited to make it clear. You may find the vitamin D council's information of interest:http://www.vitamindcouncil.org/about-vitamin-d/vitamin-d-deficiency/am-i-vitamin-d-deficient/
Thanks. Units are important especially in vitamin d where two different units are commonly used. It is important that people are encouraged to use units correctly. I saw a journal paper that used ng/dL for 25(OH)D except that the numbers were what you expected for ng/mL. I have no idea how it got past the referees.
Thanks. This is one subject where units are critical.
"Please note vD supplements should not be taken with calcium supplements as this can result in hypercalcaemia or high blood calcium levels."I question this statement, in the Burton et al 2010 study 1200 mg calcium per day was prescribed in combination with high doses vD and no side effects were reported. One definitely should not take too much calcium, but no calcium supplements is probably not enough. Hunter-gatherers ate a different diet. It might be important to measure 25(OH)D, calcium and parathyroid hormone (PTH) levels in MSers if you are worried about Bone Mineral Density in MSers.
More about vD and CalciumPlease read this:Is High Dose Vitamin D Harmful?Sanders KM, Nicholson GC, Ebeling PR.Calcif Tissue Int. 2012 Dec 19. [Epub ahead of print]PMID:23250508
What I am really getting at is to try an avoid the combined vD/Calclium supplements; these typically have only 400IU of vD per tablet – to get 5,000U you need to take excessive calcium.
You are so right.And one shold take at least 500 mg extra calcium à day.Difficult to correct, should have been should.
Low 25(OH)D causes an increase in the parathyroid hormones and this increases the blood 1,25(OH)D (active vitamin d) level, which then causes the blood calcium levels to increase (the effect is known as secondary parathyroidism). Increasing vitamin d intake lowers both the parathyroid hormones and the blood levels of 1,25(OH)D stabilising the calcium level in the blood. Taking extra calcium is not good for anyone who already has raised blood calcium levels, if it is controlled correctly it will not be a problem. Even at toxic levels of 25(OH)D the level of the active version 1,25(OH)D do not rise. The only know toxic effect of high levels of vitamin d is on the blood calcium levels so if they are normal then there is no toxicity. This is all in the New England Journal of Medicine article (2007)by Holick
What I forgot to mention is, I agree with you that tablets with 400IU and calcium should be avoided. Also as there are no known cases of toxicity at 10,000IU a day in adults why not just take that and get your doctor to check your calcium levels. They should do this anyway in case you have primary parathyrodism, sarcoidosis or certain types of lymphoma, which deregulate the blood 1,25(OH)D levels.
If this appears twice sorry I published it with one browser and it just disappeared. Low 25(OH)D causes an increase in the parathyroid hormones and this increases the blood 1,25(OH)D (active vitamin d) level, which then causes the blood calcium levels to increase (the effect is known as secondary parathyroidism). Increasing vitamin d intake lowers both the parathyroid hormones and the blood levels of 1,25(OH)D stabilising the calcium level in the blood. Taking extra calcium is not good for anyone who already has raised blood calcium levels, if it is controlled correctly it will not be a problem. Even at toxic levels of 25(OH)D the level of the active version 1,25(OH)D do not rise. The only know toxic effect of high levels of vitamin d is on the blood calcium levels so if they are normal then there is no toxicity. This is all in the New England Journal of Medicine article (2007)by Holick
The same size doesn't always fit all..I think it's really important to measure your vitD levels and then make decisions on how much to take. I have a friend who is well above 100 nanomol/litre taking only 1000 IU while I had just under 80 nanomol/litre taking 4000 IU. Where I live my neuro is not so keen on measuring my vitD-level as he seems to think it's of no importance for my MS. I had to ask my GP..I really believe it should be measured on a regular basis and the result stored in our national MS data base. Because otherwise, how are we to know.//Sara
The economics of vD testing, etc. is a problem when you are talking about population supplementation. I will post more on this. Bruce Hollis, one of the world's vD gurus, has stated that it is best to supplement yourself at a particular dose for 6-8 weeks and then test yourself to see if you need to adjust your level of supplementation. He feels there is little utility in showing that your levels are low before supplementation.
It's recommended to take vit. K2 when taking high doses of D3:http://articles.mercola.com/sites/articles/archive/2012/12/16/vitamin-k2.aspx
High Vitamin D levels may reduce the risk of relapses and disease progression in MS.Higher vitamin D levels were associated with lower, but not statistically significant, relapse risk.